SSG Case Series Review
Overview: The Use of Real-Time Intraoperative Imaging to Gain GTR
This is a 4-patient case series involving one primary tumor and three secondary tumors ranging from <1cm - 3cm. The lesions were located in the temporal, frontal and occipital lobes and the cerebellum. All surgeries were performed using a parafascicular surgical approach that involved: trajectory planning, navigation, trans-sulcal access with a tubular retractor, automated resection, exoscopic visualization, and intra-operative ultrasound. Intra-operative ultrasound is new technology for use with the tubular retractor system to localize the tumor and confirm extent of resection, which assisted in a gross total resection in 3 of the 4 cases in this series.
Clinical Presentation, Surgical Management, and Clinical Outcomes
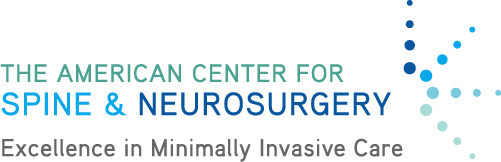
Case 1: Metastatic renal cell carcinoma
Patient is a 59-year-old female with a history of renal cell carcinoma. She presented with a complaint of numbness. Pre-op scan showed a small (<1cm) mass. Due to the small size of the tumor, potential shifting of the brain was considered during access. Cannulation was superior to the tumor to avoid displacement, but upon decoupling the access device, the tumor was not visible. Intra-operative ultrasound was introduced to locate the mass. Once identified, the lesion was resected and ultrasound was used to confirm gross total resection prior to dosing. The patient was discharged post-op day 5. Numbness resolved post-surgery.
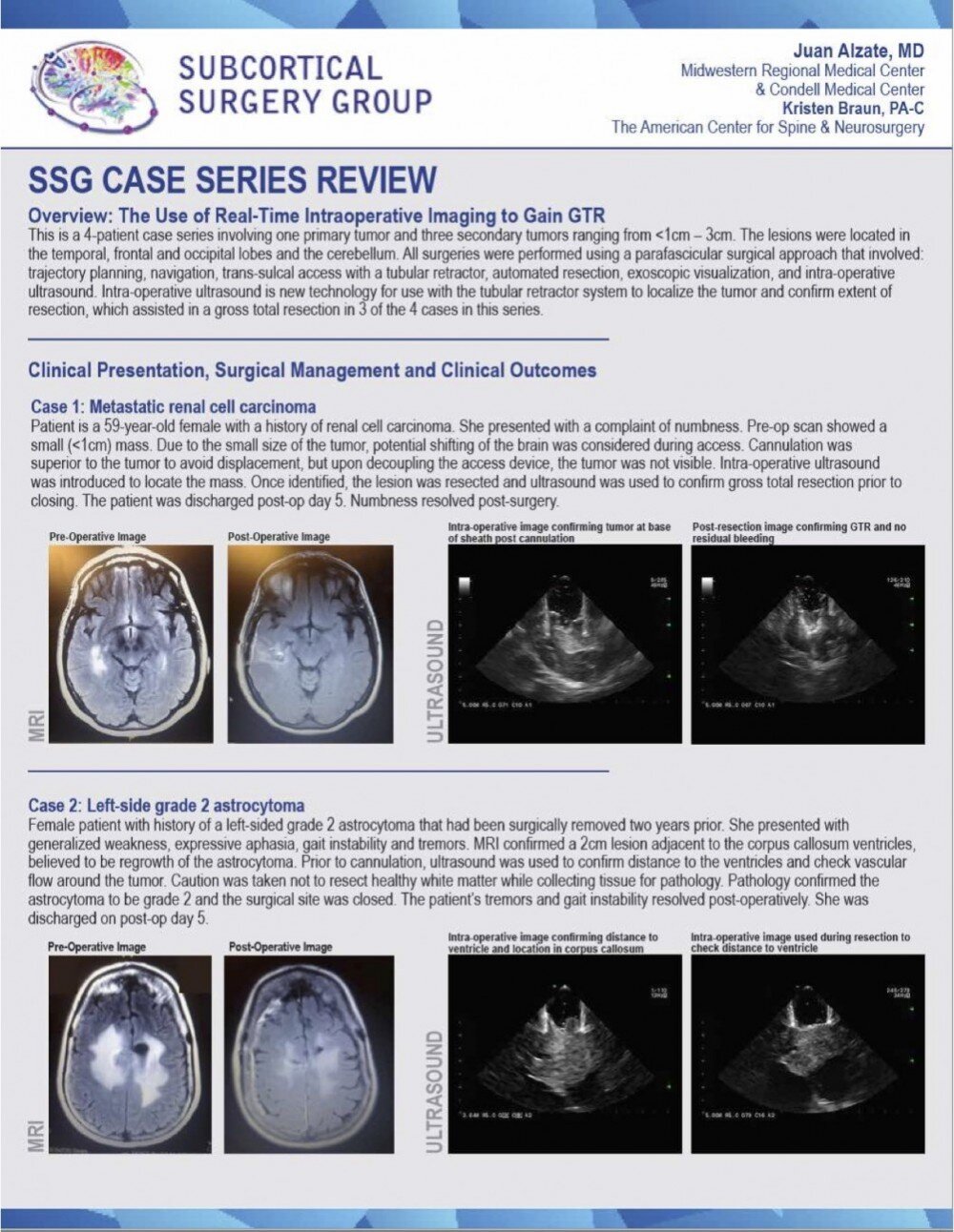
Case 2: Left-side grade 2 astrocytoma
Female patient with history of a left-sided grade 2 astrocytoma that had been surgically removed two years prior. She presented with generalized weakness, expressive aphasia, gait instability and tremors. MRI confirmed a 2cm lesion adjacent to the corpus callosum ventricles, believed to be regrowth of the astrocytoma. Prior to cannulation, ultrasound was used to confirm distance to the ventricles and check vascular flow around the tumor. Caution was taken not to resect healthy white matter while collecting 'tissue for pathology. Pathology confirmed the astrocytoma to be grade 2 and the surgical site was closed. The patient's tremors and gait instability resolved post-operatively. She was discharged on post-op day 5.
Case 3: Metastatic lung cancer
Patient is a 50-year-old male with a history of lung cancer. He presented with progressive headaches and visual changes. MRI confirmed a 2cm x 3cm mass. Based on scan interpretation, a posterior cannulation was planned to run parafascicular to major white matter tracts. During cannulation, the tumor displaced anteriorly; intra-operative ultrasound was introduced to identify the adjusted location of the tumor. Throughout resection, ultrasound was used to confirm mass location and distance from the ventricle until gross total resection was achieved. After surgery, the patient's headaches resolved and visual improvements were noted. He was discharged on post-op day 3.
Case 4: Metastatic cerebellar colon cancer
Patient is a 31-year-old male with a history of colon cancer. He presented with confusion and vertigo. MRI confirmed a 2.6cm cerebellar mass. Ultrasound was used prior to dural opening to locate tumor and confirm depth. Ultrasound also highlighted a capsule with cystic components inside the tumor. Due to the firm capsule, a surface cannulation was planned to avoid displacing the mass. Once resection was complete, ultrasound was used to confirm no residual bleeding prior to dosing. Pre-surgical symptoms resolved. The patient's ICU LOS was one day.
The details and associated images and/or videos of these clinical cases are used with permission by the surgeon and are for illustrative purposes only. © 2016.